I distinctly remember staring down at those bold pink lines and the sound of my friends eagerly jumping on the other side of the bathroom door. I ran out to join them happily screaming with joy.
Over the next few months, my husband and I prepared for parenthood and grew more in love with our son every day. My family and friends threw me an extravagant baby shower. I was blessed with a smooth delivery (shout out to midwives). I continued to work in the ICU and just knew my child would have so many loving aunties ready to take him at a moment’s notice should I ever need a break.
Did I mention we also were anticipating a move shortly after giving birth?
When we brought baby home, people came by to see him, and my husband was on paternity leave so I wasn’t overwhelmed. However, as many parents will tell you, the hype of a new baby wears off. I found myself two states away, alone, with zero coping skills and no community. I was hit with the new reality of being a stay-at-home mom. My husband was constantly gone. That support system that constantly asked about baby and me disappeared.
All that was left in our two-bedroom apartment was my infant, my thoughts, and me.
At a routine pediatric appointment, I filled out the Edinburgh Postnatal Depression Scale, a test to screen for PPD. The questions ask about your ability to laugh and see the funny side of things, your ability to look forward to things with enjoyment, and how often you blame yourself for things. Interestingly enough, I answered truthfully, but the nurse advised me to change my answers because “people are going to want to look further into that.” So I changed my answers.
Did you know that your baby will see the doctor on average six times in the first few months of life? However, postpartum moms will receive only one physical checkup approximately six weeks postpartum.
Did she assume I was just a new mother experiencing “baby blues”? Looking back, I never should’ve changed my answers. Unfortunately, I wasn’t experiencing baby blues. I was encountering the start of my journey with postpartum depression. According to the American College of Obstetrics, “baby blues” occurs about 2-3 days after childbirth and doesn’t require treatment. However, postpartum depression requires treatment via talk therapy or medication and interferes with daily living.

Factors that contribute to the likelihood of having PPD (postpartum depression) are a history of depression, lifestyle stressors, hormone level changes, and adjustment after having a baby.
» » » » » » » » » » » » » RELATED READ: Surviving the Fourth Trimester « « « « « « « « « « « « «
Now let’s zoom back to my first month after having my son. A new state, new baby, new apartment, and no support system. I noticed the hours turn into days and then weeks. I noticed I was having intense intrusive thoughts. I’d cry often. And I felt like I was a horrible mother, inadequate, and full of anxiety.
I would literally dread getting out of bed, but I still felt an immense love for my child. It’s a complicated place to be.
I was also affected by mood swings combined with bouts of sadness to the point that I couldn’t shower or eat full meals regularly. If you are seeing yourself in my story, know that there is no shame in seeking help. As soon as I let go of the stigma of having a mental illness as a mother, I’ve never felt more free. In no way does PPD mean you’re weak, a horrible mother, or you did something to cause PPD.
If you had diabetes, would you delay care to get back on track just because your neighbors would judge you? Whether you take medication or go to talk therapy, what matters is you’re taking care of yourself.
Here are some El Paso resources right in our community:
- Emergence Health Network Crisis Hotline: 915-779-1800
- Mental Health Texas: 211 Option 8
- Texas Veterans Network 1-888-737-3112
- Suicide and Crisis Hotline: 988
Another option is to talk to your primary doctor, find a telehealth option, or go to the public health department.
What’s talk therapy?
You’ll speak with a licensed professional about your situation. You might discuss role transition, grief, your relationships, stressors, and coping methods. During talk therapy which can last weeks to months, you gain more insight into the “why” and develop strategies to recover including emotional regulation. It’s worth its weight in gold to have an objective confidential party to talk to.
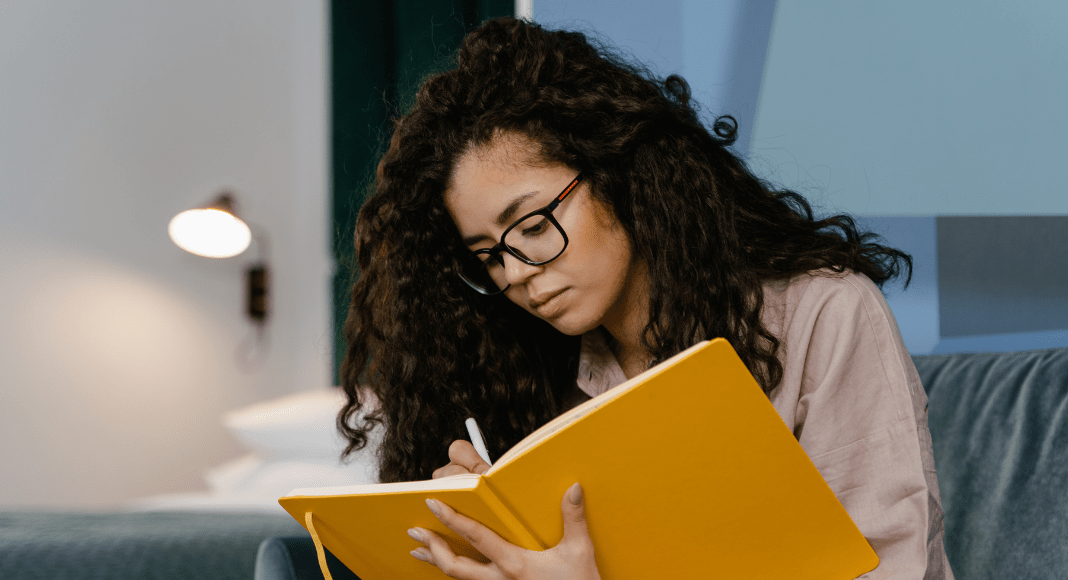 It’s been six years. With consistent work and staying on top of my symptoms, I was able to recover from PPD and also work on my battle with chronic depression. The most helpful things for me are regular talk therapy, journaling, and getting outside. I even joined a workout group and make a point to spend at least 20 minutes outside a day which helped me so much!
It’s been six years. With consistent work and staying on top of my symptoms, I was able to recover from PPD and also work on my battle with chronic depression. The most helpful things for me are regular talk therapy, journaling, and getting outside. I even joined a workout group and make a point to spend at least 20 minutes outside a day which helped me so much!
It can be difficult navigating motherhood but you CAN do this. There’s no shame in getting help. You matter. Postpartum depression does not define your worth as a person or a mother.
The opinions expressed in this post are those of the author. They do not necessarily reflect the official policy or position of El Paso Mom, its executive team, other contributors to the site, its sponsors or partners, or any organizations the aforementioned might be affiliated with.